This evidence-based‚ criterion-based protocol guides both clinicians and patients through conservative shoulder dislocation rehabilitation. It progresses through three stages‚ focusing on restoring function‚ minimizing pain‚ and preventing recurrence.
1.1 Overview of Shoulder Dislocation and Rehabilitation
Shoulder dislocation‚ commonly affecting the anterior region‚ is a frequent injury requiring structured rehabilitation. The protocol involves three stages‚ starting with immobilization and progressing to active exercises. Early immobilization for first-time dislocators (4-6 weeks) is often recommended‚ while recurrent cases may begin therapy immediately. Rehabilitation aims to restore range of motion‚ reduce pain‚ and strengthen muscles. Pain serves as a guide for progression‚ with exercises tailored to individual recovery. Physical therapy plays a central role‚ focusing on isometrics‚ mobility‚ and gradual strengthening. The goal is to enhance shoulder stability‚ prevent recurrence‚ and return patients to normal activities. A criterion-based approach ensures personalized care‚ adapting to patient needs and progress.
1.2 Importance of a Structured Rehabilitation Protocol
A structured rehabilitation protocol is crucial for optimal recovery after a shoulder dislocation. It ensures a systematic approach‚ minimizing complications and recurrence risks. By following a criterion-based plan‚ patients progress at their own pace‚ guided by clinical milestones rather than fixed timelines. This approach reduces the likelihood of premature activity that could reinjure the shoulder. Early stages focus on pain management and basic mobility‚ while later phases incorporate strengthening and functional movements. A structured protocol also enhances patient compliance and therapist accountability‚ ensuring targeted exercises and modalities are applied effectively. Ultimately‚ it supports a safer return to daily activities and sports‚ minimizing long-term instability and promoting lasting shoulder health.
Phases of Shoulder Dislocation Rehabilitation
The rehabilitation process is divided into three distinct phases‚ each addressing specific goals such as pain reduction‚ mobility restoration‚ and functional recovery to ensure a safe return to activity.
2.1 Phase 1: Immediate Post-Injury (0-4 weeks)
This initial phase focuses on pain management‚ immobilization‚ and basic exercises to prevent further injury. A sling is often used to immobilize the shoulder‚ except during hygiene or exercises. Goals include reducing inflammation and maintaining basic range of motion. Isometric exercises for the deltoid and periscapular muscles are introduced to prevent atrophy. Gentle exercises like elbow‚ wrist‚ and hand movements are encouraged to maintain mobility without stressing the shoulder joint. Pain is used as a guide to avoid overexertion. Patients may begin with passive or active-assisted range of motion exercises if tolerated. This phase lays the foundation for gradual recovery‚ with progression based on individual healing and comfort levels.
2.2 Phase 2: Restoring Mobility (4-12 weeks)
During this phase‚ the focus shifts to gradually restoring shoulder mobility and strength. Patients transition from passive to active exercises‚ incorporating gentle stretching and controlled movements. The sling may be weaned off as comfort allows‚ enabling more dynamic exercises. Emphasis is placed on improving range of motion through activities like shoulder external rotations and scapular exercises. Strengthening exercises for the rotator cuff and scapular stabilizers are introduced to enhance joint stability. Pain-free movements are prioritized‚ and exercises are progressed based on individual tolerance and healing. Manual therapy‚ such as joint mobilizations‚ may be incorporated to address any residual stiffness. This phase aims to restore functional mobility‚ preparing the shoulder for more advanced strengthening in the next phase.
2.3 Phase 3: Strengthening and Return to Activity (3-12 months)
This phase focuses on advanced strengthening and functional activities to prepare the shoulder for full return to activity. Patients progress to dynamic and resistive exercises‚ such as weighted shoulder rotations and plyometric drills‚ to enhance strength and stability. Functional movements like overhead reaching and sport-specific actions are reintroduced‚ ensuring the shoulder can handle daily or athletic demands. Supervised physical therapy continues to refine technique and address any lingering limitations. The goal is to restore pre-injury function‚ with progression tailored to the patient’s needs and goals. This phase is critical for preventing recurrence and ensuring a safe transition back to normal activities or sports‚ typically within 6-12 months post-injury.

Exercises and Activities in the Rehabilitation Protocol
The protocol includes a structured progression of exercises‚ starting with isometrics and range of motion‚ advancing to strengthening‚ and finally incorporating dynamic and functional movements to restore full shoulder function and stability.
3.1 Early Stage Exercises (Isometrics and Range of Motion)
In the initial phase‚ exercises focus on maintaining shoulder mobility and strength without causing further injury. Isometric exercises‚ such as shoulder blade squeezes and deltoid contractions‚ are performed to minimize atrophy. Patients are also guided through gentle range-of-motion exercises‚ including passive and active-assisted movements‚ to restore joint mobility without aggravating the injury. These exercises are typically done 2-3 times daily and are essential for laying the foundation for more advanced rehabilitation. Pain-free movements are emphasized to ensure proper healing and prevent recurrence of dislocation. Supervised physical therapy sessions are recommended to monitor progress and adjust the exercise program as needed. Consistency and adherence to the protocol are crucial during this stage to achieve optimal recovery outcomes.
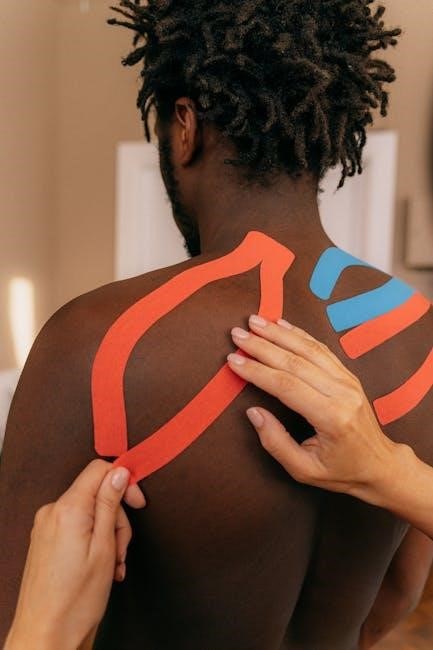
3.2 Intermediate Stage Exercises (Progressive Strengthening)
During the intermediate phase‚ the focus shifts to progressive strengthening to enhance shoulder stability and function. Patients engage in resistance band exercises‚ such as external rotations and scapular pushes‚ to target the rotator cuff and surrounding muscles. Strengthening exercises for the deltoid‚ trapezius‚ and rhomboid muscles are also introduced to improve joint stability. Dynamic movements‚ like controlled arm raises and wall slides‚ are incorporated to gradually increase range and strength. These exercises are typically performed 2-3 sets of 10-12 repetitions‚ 3-4 times per week. Progression is based on pain-free tolerance and functional improvement‚ ensuring a safe transition to more advanced activities. Supervised therapy sessions help refine technique and prevent overloading of the shoulder joint.
3.3 Advanced Stage Exercises (Dynamic and Functional Movements)
In the advanced stage‚ dynamic and functional movements are introduced to restore full shoulder function and prepare for return to activity. Exercises include plyometric drills‚ controlled overhead movements‚ and sport-specific actions to enhance proprioception and reaction time. Patients perform agitation exercises‚ such as rapid alternating arm movements‚ to improve joint stability and neuromuscular control. Functional tasks‚ like carrying objects or simulated work/sport activities‚ are incorporated to mimic real-life demands. These exercises are progressed gradually‚ ensuring pain-free and stable movement patterns; Supervised therapy sessions focus on refining technique and advancing resistance or complexity as tolerated. This phase emphasizes transitioning to unrestricted‚ dynamic movements‚ preparing the shoulder for full functional recovery and return to pre-injury activities.

Pain Management and Modalities
Pain management incorporates ice therapy‚ analgesics‚ and physical therapy modalities to reduce discomfort and inflammation. Early pain-free exercises promote healing while avoiding further injury or instability.
4.1 Role of Pain in Rehabilitation Progression
Pain serves as a critical indicator in guiding the progression of shoulder dislocation rehabilitation. It helps determine the appropriate intensity and timing of exercises‚ ensuring safe advancement through recovery phases. Clinicians monitor pain levels to adjust treatment plans‚ avoiding activities that exacerbate discomfort. Patients are advised to use pain as a guide‚ stopping exercises that cause significant distress. This approach minimizes the risk of re-injury while promoting gradual healing and strength restoration. Effective pain management strategies‚ including ice therapy and medication‚ are integrated to support a smooth transition through each rehabilitation stage‚ fostering optimal recovery outcomes and long-term shoulder stability.
4.2 Use of Ice‚ Medication‚ and Physical Therapy Modalities
The integration of ice‚ medication‚ and physical therapy modalities plays a pivotal role in managing pain and inflammation during shoulder dislocation rehabilitation. Ice therapy‚ applied in the acute phase‚ reduces swelling and alleviates discomfort. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to control pain and inflammation. Physical therapy modalities such as electrical stimulation and ultrasound are employed to enhance tissue repair and improve joint mobility. These methods are tailored to individual patient needs‚ ensuring a comprehensive approach to pain management and facilitating a smoother recovery process. Their combined use supports the restoration of shoulder function and stability‚ promoting an effective return to daily activities and sports.

Role of Physical Therapy in Rehabilitation
Physical therapy is crucial for restoring shoulder function‚ reducing pain‚ and preventing recurrence. It involves supervised exercises‚ manual techniques‚ and progression based on individual recovery.
5.1 Importance of Supervised Physical Therapy Sessions
Supervised physical therapy sessions are crucial for ensuring proper technique‚ safety‚ and progression in shoulder dislocation rehabilitation. A therapist provides personalized guidance‚ addressing specific deficits and promoting optimal recovery. They tailor exercises to individual needs‚ monitor progress‚ and adjust the program as necessary. Supervised sessions also help prevent complications‚ such as improper healing or recurrent instability. Regular therapist feedback ensures exercises are performed effectively‚ maximizing strength and mobility gains. This structured approach minimizes the risk of further injury while accelerating the return to normal function and activities. Supervised care is essential for achieving long-term stability and reducing the likelihood of future dislocations.
5.2 Individualized Progression Based on Patient Needs
Rehabilitation protocols must be tailored to each patient’s unique condition‚ goals‚ and progress. A one-size-fits-all approach is ineffective‚ as recovery varies based on factors like age‚ activity level‚ and injury severity. Individualized progression ensures exercises and therapies are adjusted to meet specific needs‚ optimizing outcomes. Clinicians assess each patient’s strength‚ range of motion‚ and pain levels to modify the program. This personalized approach minimizes risks of overexertion or underperformance‚ ensuring safe and efficient recovery; Regular reassessments allow for timely adjustments‚ keeping patients on track to achieve their functional goals. Personalized care enhances adherence and motivation‚ leading to better overall results and faster return to daily activities or sports.
